Many eye problems come with advancing age. Presbyopic, the need for reading glasses, is inevitable. Other examples include cataract, glaucoma, age related macular degeneration, diabetic retinopathy.
The risks of having eye diseases increase with a positive family history, hypertension, cardiovascular diseases, diabetes, smoking and alcohol abuse.
People over age 55 years are recommended to have regular eye check up every one or two years in order to initiate treatment during the early stages of the disease.
An opacified lens in the eye is a cataract. The eye is similar to a camera, light rays are focused by the lens onto the retina in order to form a sharp image. When a lens becomes opacified, the image formed will be blurred. The commonest cause of cataract is aging; other causes include diabetes, trauma, inflammation and congenital.
Most patients with cataracts will notice gradual blurring of vision. Others symptoms include glare under bright light, double vision in one eye, frequent change of glasses prescriptions, reduced dependence on reading glasses. The eye is not painful nor red unless in advanced cases with complications.
While some medications may slow down cataract development, in order to prevent cataract formation one should avoid strong ultra-violet light exposure by the use of sunglasses.
Surgery is the only treatment for cataract, and over 95% of patients can restore their vision after surgery. After the removal of cataract, an individualised intraocular lens implant will be fitted in place for best visual outcome. Usually this microscopic surgery is performed under local anesthesia and lasts less than 30 minutes. There is no need to stay in the hospital after surgery. Most cataract are removed by ultrasound phacoemulsification. This minimally invasive approach ensures faster recovery due to a small wound size.
No, this approach is outdated. As the outcome for cataract surgery is excellent nowadays, the timing is based on visual needs. When eyesight has effected the activities of daily living, then cataract surgery should be considered.
Some patients experience visual deterioration a few years after cataract surgery. When a cataract was removed, its transparent capsule was left intact in order to support the intraocular lens implant. In some cases, the capsule may become opacified or scarred with time and vision is then affected. The opacified capsule can be treated with a simple laser procedure call Nd:Yag capsulotomy, after which lights rays can again be focused sharply on the retina forming a clear image.
Normal
Glaucoma
Glaucoma is usually caused by elevated intraocular pressure leading to visual loss.
When the drainage channels are blocked, fluid trapped inside the eye leads to elevated intraocular pressure. Such pressure damages the optic nerve fibres causing irreversible visual deterioration and ultimately blindness.

Normal

Glaucoma
Normal

Floaters
Floaters are sometimes described as seeing black spots. While they can be caused by different diseases, the majority is due to vitreous condensation. The vitreous body is a transparent gel - like substance filling up the space between the lens and the retina; light rays pass through the vitreous and project onto the retina. With advancing age, the vitreous body contracts and detaches itself from the surface of the retina. Additionally the vitreous body may develop opacities during this condensation process which form shadows onto the retina. These can be seen as dots, lines, small patches or spider webs. On the other hand, vision threatening diseases such as retinal tear, retinal detachment, vitreous haemorrhage, uveitis can present with similar floaters. Therefore prompt examination by an experienced ophthalmologist is recommended.
Though most floaters are benign and may become less apparent overtime, there are some medications that may reduce the vitreous condensations.
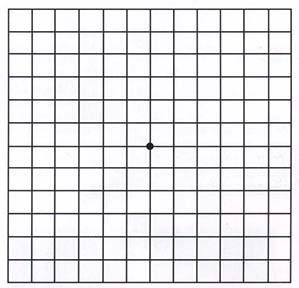
The central region of the retina is the macula. When there is pathological changes in the macula, central vision will be distorted and blurred. In maculopathy, fine vision and reading will be affected most, while peripheral vision is preserved. Frequently such changes are related to ageing, where it is known as age related macular degeneration. Age related macular degeneration usually occurs after the age of 50, and it is a major cause of permanent blindness after the age of 60. At the early stages, the symptoms experienced may not be very obvious. If the maculopathy is the educative type however, vision may deteriorate rapidly during the two years after diagnosis, leading to blindness.
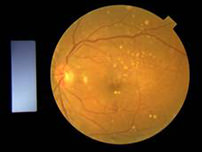
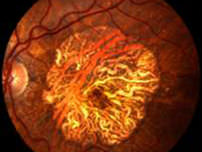

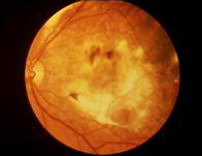
It is usually found in patients over the age of 50, more with advancing age, but no sexual predominance. The retinal degenerates with thinning causing deterioration of macular function. Possible factors include familial history, dietary habit, smoking, exposure to excessive radiation, cardiovascular diseases and anxiety.
One of the treatment is by photodynamic therapy. A photosensitizing agent is injected which will attach onto the abnormal blood vessels. A low energy laser is then applied locally onto the affected area, and those treated abnormal vessels will stop growing and leaking. The advantages are that there is no damage to the retina and there is no scar formation.
Anti-VEGF injection have been shown to be effective in treating AMD. These injections are usually administered in our day surgery centre, while the injections are given in a sterile and clear setting. Monthly injection schedules are usually tailored-made to the patients conditions in order to achieve the maximum benefits of the anti-VEGF therapy.

Normal

Retinal Detachment

retinal detachment
When the vitreous humour contracts, it may cause breaks in the retina. When fluid seeps under the retina through these retinal breaks, the retina will become detached.
During the acute phase of a retinal detachment, the patient may experience:
Retinal detachment cannot be prevented by medication. If retinal breaks are recognised early by an ophthalmologist through examination with pupil dilation, laser barrier or cryotherapy may be applied to seal off such breaks, thereby prevent the development of retinal detachment. Therefore the most effective prevention is to be aware of the warning signs such as floaters and light flashes, and seek the help of an ophthalmologist promptly for a complete eye examination. For those with severe short-sightedness, it is advisable to avoid contact sports and have regular check ups.


Retinal detachment is a serious situation, and surgery to repair retinal detachment is complicated. The success rate may be up to 90%, but multiple surgeries are at times required. There are basically two categories of surgeries: by the insertion of an explants onto the sclera in the form of a silicone band or buckle then application of cryotherapy to the retinal breaks, or by pars plana vitrectomy where the laser is applied to seal off the retinal breaks and gas may be injected in place of the vitreous removed in order to flatten the retina.